Introduction
A heart attack 2014, medically known as a myocardial infarction (MI), is a serious and potentially fatal condition that occurs when the blood supply to a part of the heart is suddenly blocked. This leads to the death of heart muscle tissue due to the lack of oxygen. Heart attacks are a leading cause of death worldwide and are commonly associated with coronary artery disease (CAD). Understanding the causes, symptoms, diagnosis, treatment, and prevention of heart attacks is critical in managing this life-threatening condition.
Causes of Heart Attacks
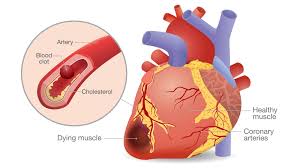
The most common cause of a heart attack is the blockage of a coronary artery due to atherosclerosis—the buildup of plaque (fatty deposits, cholesterol, and other substances) on the inner walls of the arteries. Over time, these plaques can rupture, forming a blood clot that obstructs the flow of blood to the heart muscle.
Other causes include:
- Coronary artery spasm: Temporary tightening of the muscles in the artery wall can reduce or completely stop blood flow.
- Coronary artery dissection: A rare condition where the layers of an artery wall tear.
- Severe anemia or low oxygen levels: These conditions can limit the oxygen supply to the heart muscle.
- Drug use: Stimulants like cocaine can cause coronary artery spasms leading to a heart attack.
Risk factors for heart attacks include:
- High blood pressure
- High cholesterol
- Diabetes
- Smoking
- Obesity
- Sedentary lifestyle
- Stress
- Family history of heart disease
- Excessive alcohol consumption
Symptoms of a Heart Attack
Heart attack symptoms can vary between individuals and may differ between men and women. Common symptoms include:
- Chest pain or discomfort: Often described as pressure, squeezing, fullness, or pain in the center or left side of the chest.
- Shortness of breath: May occur with or without chest discomfort.
- Pain or discomfort in other areas: Such as the arms, back, neck, jaw, or stomach.
- Cold sweats
- Nausea or vomiting
- Lightheadedness or sudden dizziness
- Fatigue
In women, symptoms may be subtler and include fatigue, indigestion, and pain in the back or jaw. Silent heart attacks, which show no obvious symptoms, can also occur, particularly in diabetics.
Diagnosis
Prompt and accurate diagnosis is crucial in treating heart attacks. Common diagnostic procedures include:
- Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart and helps detect abnormalities indicative of a heart attack.
- Blood tests: Specifically for cardiac enzymes like troponin, which are released into the blood when heart muscle cells are damaged.
- Chest X-ray: Helps rule out other causes of chest pain.
- Echocardiogram: An ultrasound of the heart that can assess the damage and function of the heart.
- Coronary angiography: A special dye and X-ray imaging technique used to view the arteries and locate blockages.
- CT or MRI scans: May be used for more detailed imaging in complex cases.
Types of Heart Attacks
There are different types of heart attacks, primarily classified based on the extent and location of blockage:
- ST-Elevation Myocardial Infarction (STEMI):
- A complete blockage of a coronary artery.
- Requires immediate intervention.
- Non-ST-Elevation Myocardial Infarction (NSTEMI):
- Partial blockage.
- Less severe than STEMI but still requires urgent medical care.
- Silent Myocardial Infarction:
- No obvious symptoms.
- Often discovered later through testing or imaging.
Treatment
Immediate treatment can save lives and minimize heart damage. The main goal is to restore blood flow to the affected heart muscle as quickly as possible.
Emergency Treatment
- CPR (Cardiopulmonary Resuscitation): If the patient is unresponsive and not breathing.
- Defibrillation: For cardiac arrest due to arrhythmia.
Medications
- Aspirin: Reduces blood clotting.
- Thrombolytics (clot busters): Help dissolve clots quickly.
- Antiplatelet agents: Such as clopidogrel.
- Anticoagulants: Reduce the formation of new clots.
- Pain relievers: Like morphine to relieve discomfort.
- Nitroglycerin: Improves blood flow to the heart.
- Beta-blockers: Slow the heart rate and decrease blood pressure.
- ACE inhibitors and statins: Improve heart function and lower cholesterol.
Surgical and Non-Surgical Procedures
- Angioplasty and stent placement: A balloon is inserted into the blocked artery to open it up, often followed by placing a stent to keep it open.
- Coronary artery bypass grafting (CABG): A more invasive procedure where blood flow is redirected around the blocked artery using a vessel graft.
Recovery and Rehabilitation
Recovering from a heart attack can take several weeks or months depending on the severity. Key components of rehabilitation include:
1. Cardiac Rehabilitation Programs
These structured programs typically involve:
- Exercise training
- Nutritional counseling
- Education about heart health
- Stress management
- Smoking cessation
2. Lifestyle Changes
- Healthy diet: Low in saturated fats, trans fats, salt, and sugar.
- Regular physical activity: At least 150 minutes of moderate exercise per week.
- Weight management
- Smoking cessation
- Limiting alcohol intake
Complications
Heart attacks can lead to serious complications, especially if not treated promptly. These include:
- Arrhythmias: Irregular heartbeats, which can be fatal.
- Heart failure: When the heart is unable to pump blood effectively.
- Cardiogenic shock: A life-threatening condition where the heart can’t supply enough blood to the organs.
- Heart rupture: A tear in the heart wall, valves, or septum.
- Pericarditis: Inflammation of the lining around the heart.
- Repeat heart attacks
Prevention

Preventing a heart attack involves managing risk factors and adopting a heart-healthy lifestyle. Key prevention strategies include:
- Controlling blood pressure and cholesterol
- Managing diabetes
- Quitting smoking
- Eating a balanced diet
- Maintaining a healthy weight
- Exercising regularly
- Limiting alcohol
- Managing stress
- Regular health check-ups
Medications like statins, antihypertensives, and aspirin (if prescribed) can also help reduce the risk of a first or recurrent heart attack.
Heart Attack Statistics and Global Impact
Heart disease remains the leading cause of death globally. According to the World Health Organization:
- Over 17 million deaths annually are attributed to cardiovascular diseases.
- Of these, nearly 85% are due to heart attacks and strokes.
- In the United States alone, someone has a heart attack approximately every 40 seconds.
The economic burden is also significant, with billions spent on healthcare costs, lost productivity, and long-term care.
Recent Advances in Treatment
Modern medicine has significantly improved the survival rate of heart attacks. Advances include:
- Drug-eluting stents: Reduce the risk of artery re-narrowing.
- Remote monitoring devices: Allow for real-time heart function tracking.
- Genetic testing: Helps predict susceptibility.
- Stem cell therapy and regenerative medicine: Experimental treatments to repair damaged heart tissue.
Emotional and Psychological Effects
Survivors of heart attacks often experience emotional challenges, including:
- Anxiety
- Depression
- Fear of recurrence
- Post-traumatic stress disorder (PTSD)
Psychological counseling, support groups, and open communication with loved ones are crucial aspects of recovery.
Conclusion
A heart attack is a life-threatening medical emergency that requires rapid intervention. Despite its severity, many individuals survive and live fulfilling lives with the help of modern medical treatment, rehabilitation, and lifestyle changes. Understanding the causes, recognizing the symptoms, and taking proactive steps to prevent a heart attack can make a significant difference in outcomes. With increased awareness and better health practices, we can reduce the global burden of heart disease and save countless lives.
Let me know if you’d like this turned into a printable PDF, or if you need references or citations added!
When someone has a heart attack, time is critical. Medications play a vital role in saving the heart muscle, preventing further damage, and improving long-term outcomes. These drugs fall into several categories, each serving a different purpose.
1. Aspirin
- Purpose: Thins the blood and prevents clots from getting worse.
- How it works: It stops platelets from sticking together.
- Given: Immediately during a heart attack and often continued long-term.
- Common brand names: Ecotrin, Bayer Aspirin
2. Thrombolytics (Clot Busters)
- Purpose: Dissolve the clot that is blocking the artery.
- When used: Within hours of the heart attack onset (ideally within 6 hours).
- Examples:
- Alteplase (tPA)
- Streptokinase
- Tenecteplase
- Important note: Not given if there’s a high risk of bleeding.
3. Antiplatelet Drugs
- Purpose: Prevent new clots from forming.
- Often used with aspirin.
- Examples:
- Clopidogrel (Plavix)
- Prasugrel (Effient)
- Ticagrelor (Brilinta)
- Used for: Both immediate treatment and long-term protection, especially after stent placement.
4. Anticoagulants (Blood Thinners)
- Purpose: Help prevent new clots from forming.
- Examples:
- Heparin (injected during hospital stay)
- Enoxaparin (Lovenox)
- Warfarin (Coumadin) – for long-term use in certain patients
- Newer options: Rivaroxaban (Xarelto), Apixaban (Eliquis)
- Used in combination with other meds in certain cases.
5. Nitroglycerin
- Purpose: Relieves chest pain (angina) by widening blood vessels.
- Forms: Pills, sprays, patches, or IV.
- Note: Only treats symptoms—not the blockage itself.
6. Beta-Blockers
- Purpose: Reduce heart workload and lower blood pressure.
- Help prevent irregular heartbeats (arrhythmias).
- Examples:
- Metoprolol (Lopressor)
- Atenolol
- Carvedilol (Coreg)
- Benefits: Lower the risk of a second heart attack and improve survival.
7. ACE Inhibitors / ARBs
- ACE Inhibitors: Help relax blood vessels and reduce heart stress.
- Examples: Lisinopril, Enalapril
- ARBs: Used if patients can’t tolerate ACE inhibitors.
- Examples: Losartan, Valsartan
- Help prevent heart failure and reduce long-term damage.
8. Statins (Cholesterol-Lowering Drugs)
- Purpose: Lower LDL (“bad”) cholesterol and stabilize plaque in arteries.
- Examples:
- Atorvastatin (Lipitor)
- Rosuvastatin (Crestor)
- Simvastatin (Zocor)
- Used long-term for secondary prevention after a heart attack.
9. Pain Relief
- Morphine: Sometimes used in hospitals to relieve severe chest pain.
- Note: Used cautiously because it can affect blood pressure.
10. Diuretics
- Purpose: Help remove excess fluid, especially if heart failure is present.
- Examples: Furosemide (Lasix), Spironolactone
Important Reminders
- Always take medications exactly as prescribed.
- Do not stop heart meds suddenly—that can be dangerous.
- Regular follow-ups and blood tests may be needed to check drug levels and effects.
- Watch for side effects like dizziness, bleeding, or swelling.
If you’re writing a report or presentation, I can help organize this into a table or add explanations about how each drug works at a molecular level. Just let me know!
4. Oxygen
- Why it’s primary: If oxygen levels are low (SpO₂ < 90%), supplemental oxygen helps improve heart muscle oxygenation.
- Note: Not given routinely unless oxygen levels are low.
5. Thrombolytics (Clot Busters)
- Why it’s critical: These dissolve the blood clot causing the heart attack.
- Used when: No access to immediate angioplasty (PCI).
- Examples: Alteplase (tPA), Streptokinase, Tenecteplase.
6. Antiplatelets (in addition to aspirin)
- Purpose: Prevent formation of new clots.
- Examples:
- Clopidogrel (Plavix)
- Ticagrelor (Brilinta)
- Prasugrel (Effient)
- Given: ASAP after diagnosis and continued after discharge.
7. Anticoagulants (Blood Thinners)
- Purpose: Prevent new clots during hospital care.
- Examples:
- Heparin (IV)
- Enoxaparin (Lovenox, subcutaneous)
- Used in: Both STEMI and NSTEMI treatment.
BONUS: MONA – Memory Trick
Doctors and nurses use the acronym MONA to remember the initial emergency medications:
- M – Morphine
- O – Oxygen
- N – Nitroglycerin
- A – Aspirin
Note: MONA is not necessarily the order of administration — aspirin usually comes first!
Very good https://shorturl.at/2breu
Good https://lc.cx/xjXBQT
Good https://t.ly/tndaA